Life with a healthcare worker in 2020
April 15, 2020

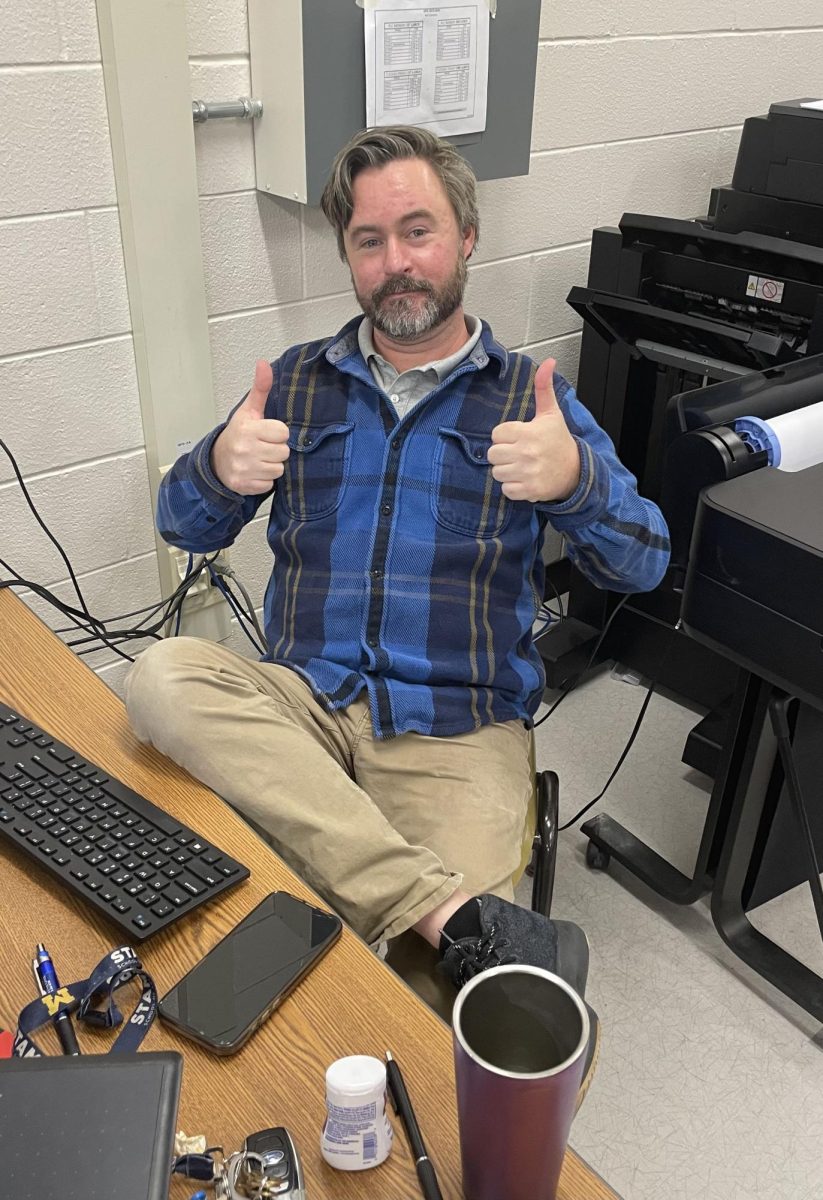
For the past eight years Jeffery James Cornell, better known as dad, has worked as a physician assistant (PA) primarily in the emergency room. His crazy work stories would always amuse me; sewing someone’s eye lid, getting kicked in the back of the head while trying to hold a patient down, and the patient who thanked him for saving his life when he saw him a couple months later.
My dad advises my entire family and some friends about medicine, and serves as a family medical expert whenever someone is ill.
Myself being a hypochondriac, I am constantly diagnosing myself with new or rare diseases and thankfully my dad has always been there to ensure that whatever new disease I think that I have, that I actually don’t’ have and explains why.
With the coronavirus, the amount of stories he shares is the same, except the stories are very different.
Instead of joking about the silly reasons some people come to the ER, like having a brown spot on your foot which was dirt, non-serious illnesses are turned away. Most hospitals have a tent in front of the entrance of the ER where a staff member will do a quick physical examination to determine if that person should be allowed inside. At Henry Ford in Wyandotte my dad has worked in the tent, turning potential patients away because they are safer to be treated at home and would actually be more at risk being in the Hospital and exposed to Covid-19.
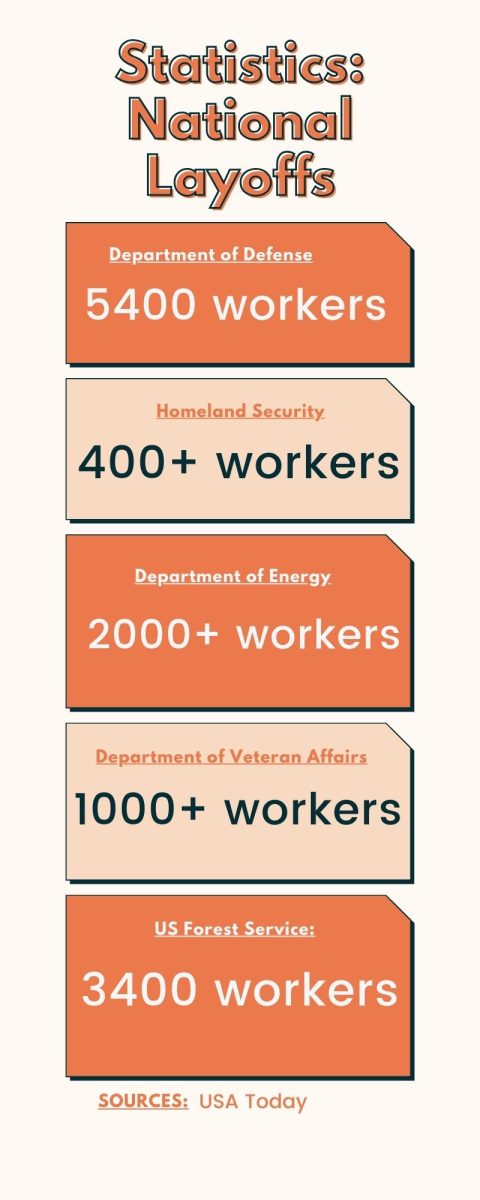
ERs and family practices are laying off workers because turning away patients has decreased the volume. Due to this, healthcare workers are forced to find a new place to work, one of my dad’s friends went to New York to work at a temporary hospital. The Cobo center is turning into a temporary hospital to tackle Covid-19, becoming a new opportunity to those laid off. Health workers are deemed essential, yet more are being laid off and the ones left are required to work extra hours.
Long hours and more shifts are only part of the problem.
The major hassle is the lack of personal protection equipment. Hospitals have started to ration; my dad has a couple of n95 masks which he now has to rotate which one he wears each day while the others hang on our coat rack to disinfect. Gowns, which used to be thrown away after seeing a patient, are now left in the patient’s room and reused for a day, they have to write their names on it so no one else uses their gown.
Anti bacterial wipes and hand sanitizer are so scarce that after receiving a donation from a school, my family immediately took it to the hospital. Despite it being a large donation my dad said that the wipes will most likely only last a week.
Recently my dad has also started working in the ICU for Ascension Macomb Hospital where he has treated Covid-19 patients. Since there is no cure at the moment, the most my dad and other healthcare workers do is support; monitor the patient’s oxygen levels, take an x-ray of their chest and readjust the ventilator as needed and wait until the patient’s immune system kicks in. A few days ago my dad would’ve said that once someone goes on a ventilator they don’t go off, however last night my dad was able to take two people off and hopefully this continues.

Because Covid-19 requires immense amounts of healthcare worker labor, Governor Whitmer just issued Executive order 2020-30 that allows PA’s, NPs, and other medical providers the ability to practice without the supervision of a doctor.
This allows flexibility for the Hospital systems to utilize medical providers from one area of the hospital that has seen decreased volumes to other areas of the hospital that have increased volume to meet the demand of this pandemic.